Background: Air pollution is associated with numerous adverse health outcomes in the general population such as asthma exacerbations, pneumonia, myocardial infarction, and stroke. There is a strong association between air pollution and mechanistic processes associated with oxidative stress, vasoconstriction, and inflammation, suggesting a high risk of exposure for those with sickle cell disease (SCD). A small number of published studies have explored this relationship, primarily focusing on children. Only two studies have examined air pollution in the US, both with outcomes among urban area hospitals in Atlanta, GA. None have taken place in California, which has the worst air quality, including the four most polluted cities in year-round particle pollution in the nation. Additionally, all published studies have overlooked more rural exposure areas. Recent advances in environmental exposure assessment have enabled high-resolution predictions of ambient air pollution concentrations in the whole US, making it possible to cover unmonitored suburban and rural areas that were unrepresented in the past. In addition, these high-resolution predictions are more precise surrogates of the personal exposure measures than monitored data. Particulate matter with a diameter of 2.5 microns or less (PM 2.5) is the most harmful pollutant based on current research findings. We hypothesized that short term increases in PM 2.5 exposure were associated with an increased risk for hospitalization among individuals with SCD in California.
Methods: We designed a time-stratified case-crossover study to estimate the percent change in risk for hospitalization for SCD complications associated with each 1mg/m 3 increase in PM 2.5 exposure. The zip code of residence was used to spatially link each hospital admission with PM 2.5 exposure using a novel hybrid exposure model allowing for estimated exposure in areas without direct remote sensing. We used conditional logistic regressions to examine the PM 2.5 exposures at 7-day moving average and single lag days (from lag 0 to 6 days) before admission, adjusting for nonlinear confounding effects of air temperature and humidity at the same exposure window. We examined risk for all hospitalizations and specifically for vaso-occlusive pain (VOC) and acute chest syndrome (ACS).
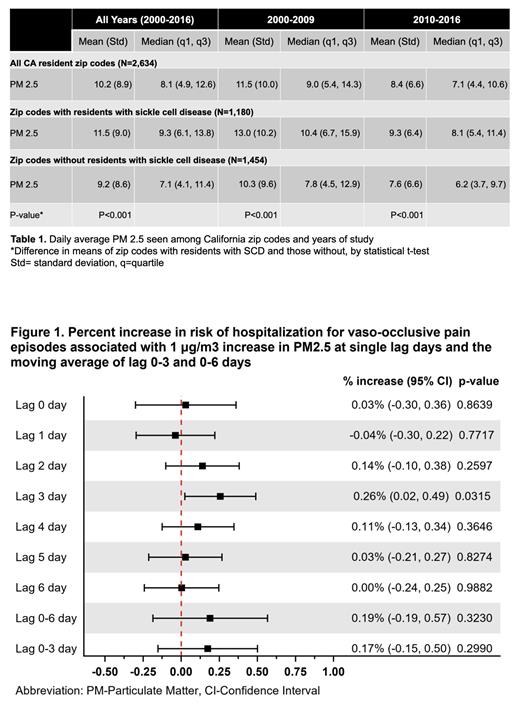
Results: From 2000-2016, among 5,835 California residents with SCD, there were 107,450 admissions for sickle cell disease complications with VOC being the most common indication (71.1%). PM 2.5 air pollution data was examined among 2,634 zip codes throughout the state. Residents with SCD were noted to be living among 1,180 zip codes. The daily burden of PM 2.5 was higher in zip codes with residents with SCD (mean 11.5 mg/m 3, standard deviation [SD] 9.0) when compared to zip codes without residents known to have SCD (mean 9.2 mg/m 3, SD 8.6, p<0.001) ( Table 1). Overall, the mean daily burden of PM 2.5 declined in the period of 2010-2016 when compared to that from 2000-2009. However, the daily mean PM 2.5 concentration remained higher in zip codes with individuals with SCD. No significant association was seen in examining the week-long exposure to PM 2.5 and increase risk in hospitalizations for any indication over the entire study period (2000-2016). However, when examining the more contemporary period of 2010-2016, we identified that each 1mg/m 3 increase in PM 2.5 was associated with 0.22% increased risk for SCD hospitalization (Confidence Interval [CI] 0.02-0.42, p=0.03) 3 days prior to admission. We observed a 0.26% increased risk for hospitalization for VOC with each 1 mg/m 3 increase in PM 2.5 exposure (CI 0.02-0.49, p=0.03) at lag day 3 (Figure 1). No effect was seen with PM 2.5 on hospitalizations for ACS during any time period.
Discussion: Our study suggests that short term air pollution exposure may be a trigger for hospitalization for individuals with SCD. In particular this effect is seen in the more recent years with a lower daily average PM 2.5 burden overall, suggesting attention may be needed well below Environmental Protection Agency (EPA) thresholds. Consistent with previous studies, lag day 3 PM 2.5 exposure is associated with an increased risk for hospitalization for VOC. These results may have important implications in understanding risk factors for hospitalization for children and adults with SCD.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal